Migraine pain is primarily caused by changes in the brain’s blood flow and nerve pathways. It is often triggered by factors such as hormonal changes, stress, certain foods, and environmental factors.
Additionally, genetics and family history can play a role in predisposing individuals to migraines. Migraine pain can vary in intensity and duration, and it is often accompanied by symptoms such as nausea, sensitivity to light and sound, and visual disturbances.
Understanding the causes of migraine pain is crucial in effectively managing and preventing migraines for those who suffer from this condition.
Understanding Migraine Pain
Migraine pain is a debilitating condition that affects millions of people worldwide. Understanding the causes and characteristics of migraine pain is crucial in managing and finding relief from this excruciating condition.
What Is A Migraine?
A migraine is a neurological disorder characterized by recurring, severe headaches that are often accompanied by other symptoms such as nausea, vomiting, and sensitivity to light and sound. It is important to note that migraines are not just ordinary headaches – they can significantly impact a person’s quality of life and daily functioning.
Characteristics Of Migraine Pain
Migraine pain is often described as throbbing or pulsating and is typically felt on one side of the head. The intensity of the pain can range from moderate to severe and can last for several hours to days. Many people also experience other symptoms along with the pain, including:
- Increased sensitivity to light, sound, and smells
- Nausea and vomiting
- Dizziness or vertigo
- Visual disturbances, such as seeing flashing lights or blind spots
- Difficulty concentrating or finding words
The Impact Of Migraine On Daily Life
Migraines can have a significant impact on an individual’s daily life. The pain and accompanying symptoms can make it difficult to perform regular activities and can interfere with work, school, and social life. Migraines can also lead to emotional distress and mental health issues, as the chronic pain and lack of control over the condition can be frustrating and distressing for those affected.
By understanding the causes, characteristics, and impact of migraine pain, individuals can better manage their condition and seek appropriate treatment. It is important to consult with a healthcare professional to develop a personalized plan for managing migraines and improving overall quality of life.
Genetic Factors And Migraine Pain
Migraine pain can be a debilitating condition that affects millions of people worldwide. While the exact cause of migraines is still not fully understood, it is believed that genetic factors play a significant role in the development of this condition.
Genetic Predisposition To Migraines
Research has shown that individuals with a family history of migraines are more likely to experience migraines themselves. This suggests that there is a genetic predisposition to migraines, meaning that certain genes may make an individual more susceptible to developing this condition.
Familial Patterns Of Migraine Occurrence
Studies have found a clear familial pattern in the occurrence of migraines. For example, if a parent suffers from migraines, their children have a higher likelihood of developing migraines as well. This suggests that there may be specific genes that are passed down from generation to generation, increasing the risk of migraines within certain families.
Genes Associated With Migraines
Researchers have identified several genes that are associated with migraines. One such gene is the MTHFR gene, which plays a role in the regulation of homocysteine levels in the body. Variations in this gene have been found to increase the risk of migraines. Another gene that has been linked to migraines is the KCNK18 gene, which is involved in the regulation of potassium channels in the brain.
Additionally, a study published in the journal Human Genetics identified a gene called TRESK that may play a role in migraine susceptibility. These genetic discoveries are providing valuable insights into the underlying mechanisms of migraines and may eventually lead to more targeted treatments.
In conclusion, genetic factors play a significant role in the development of migraines. Familial patterns of migraine occurrence and the identification of specific genes associated with migraines provide evidence for a genetic predisposition to this condition. Continued research in this field will help unravel the complex relationship between genetics and migraines, ultimately leading to better understanding and management of this often debilitating condition.
Environmental Triggers Of Migraine Pain

Migraine pain can be debilitating, impacting the quality of life for those who suffer from it. While the exact causes of migraines are not fully understood, there are environmental factors known to trigger or exacerbate migraine attacks. Understanding these triggers is key to managing and preventing migraines. In this article, we will explore common environmental triggers of migraine pain and their effects on individuals. By identifying these triggers, individuals can take proactive steps to reduce the likelihood of experiencing a migraine.
Common Triggers Like Stress And Lack Of Sleep
Stress and lack of sleep are two of the most common triggers for migraines. Both physical and emotional stress can lead to an increased risk of migraine attacks. When we experience stress, our bodies release chemicals that can trigger a migraine. Similarly, inadequate sleep or poor sleep quality can disrupt the brain’s normal functioning and make individuals more susceptible to migraine pain.
To reduce the impact of stress on migraines, it is important to incorporate stress-relieving techniques into daily routines. This may include practising relaxation exercises, such as deep breathing or meditation, or engaging in activities that promote a sense of calm and well-being. Additionally, establishing a regular sleep schedule and prioritizing quality sleep can help minimize the risk of migraines triggered by sleep deprivation.
Dietary Triggers And Their Effects On Migraines
The foods we consume can also play a significant role in triggering migraines. Certain foods and beverages, such as aged cheese, processed meats, chocolate, caffeine, and alcohol, are known to trigger migraines in some individuals. These triggers can vary from person to person, so it’s important to keep a migraine diary to identify which foods may be causing your migraines.
Avoiding trigger foods and maintaining a healthy, well-balanced diet can help reduce the frequency and severity of migraines. Including plenty of fruits, vegetables, whole grains, and lean proteins in your diet can provide essential nutrients and support overall brain health. Additionally, staying hydrated throughout the day by drinking an adequate amount of water can also help prevent migraines.
The Role Of Weather Changes In Triggering Migraines
Changes in weather conditions, particularly shifts in temperature, humidity, and barometric pressure, have long been associated with migraines. While the exact mechanisms behind this relationship are not fully understood, it is believed that these weather changes can trigger chemical and neurological responses in the brain, leading to migraine attacks.
Individuals who are sensitive to weather changes should closely monitor weather forecasts and take precautionary measures to manage their migraines. This may include wearing sunglasses to protect against bright sunlight, using earplugs to minimize sensory overload during thunderstorms, or using air purifiers to decrease exposure to potential allergens in the air.
By recognizing and addressing environmental triggers, individuals can take control of their migraines and work towards preventing future episodes. Whether it is managing stress, adopting a healthy diet, or preparing for weather changes, proactive measures can make a significant difference in reducing the impact of migraines on daily life.
Hormonal Factors And Migraine Pain
Hormonal factors play a significant role in causing migraine pain. Fluctuations in hormone levels can trigger and worsen migraines in many individuals. Understanding the influence of hormones on migraines can help us explore effective prevention and treatment strategies.
The Influence Of Hormones On Migraines
Hormones are chemical messengers in the body that regulate various physiological processes. They can have a profound effect on the occurrence and severity of migraines. Women, in particular, may be more susceptible to hormonal migraines due to the complex interplay between hormones and neurotransmitters.
There are several hormonal factors that can contribute to migraine pain:
Migraines And The Menstrual Cycle
Many women experience migraines that are closely tied to their menstrual cycle. These migraines often occur in relation to hormonal changes during the different phases of the cycle. They may be triggered by estrogen withdrawal that happens just before menstruation or by the rapid increase in estrogen levels during ovulation. Estrogen plays a critical role in modulating the sensitivity of the brain to pain, making women more susceptible to migraines during specific times of their cycle.
During menstruation, hormonal changes can cause inflammation and constriction of blood vessels, leading to migraines. The drop in estrogen levels is thought to trigger a series of chemical reactions that activate the pain pathways in the brain.
Similarly, migraines can occur during the perimenopause and menopause phases when hormone levels fluctuate drastically. The declining levels of estrogen and progesterone during menopause can increase the frequency and intensity of migraines in some women.
Pregnancy And Migraines
Pregnancy is another period where hormonal changes can impact migraines. For some women, pregnancy provides relief from migraines, especially during the second and third trimesters. The high levels of estrogen and progesterone during pregnancy may have a protective effect on migraines, reducing their frequency and severity.
However, not all women experience improvement in migraines during pregnancy. In some cases, hormonal changes and fluctuations can actually trigger migraines or make them worse. It is important for pregnant women who suffer from migraines to consult with their healthcare provider for appropriate management strategies that are safe during pregnancy.
Understanding the influence of hormonal factors on migraines is crucial for effective management and prevention. By recognizing the patterns and triggers associated with hormonal migraines, individuals can make lifestyle modifications, use medication therapies, and explore hormonal treatments that can help reduce the frequency and intensity of migraine pain.
Neurological Causes Of Migraine Pain
Migraines, those excruciating headaches that can disrupt our daily lives, have long been a subject of study and investigation by medical professionals. One key aspect of migraines is their neurological origin. Understanding the neurological causes of migraine pain can provide us with valuable insights into the underlying mechanisms that contribute to this debilitating condition.
Abnormal Brain Activity And Its Link To Migraines
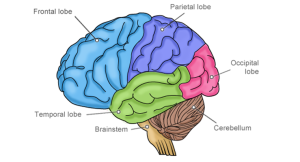
In the realm of neurological causes, abnormal brain activity has been identified as a significant factor in triggering migraines. The brains of individuals who experience migraines have been found to exhibit distinct patterns of abnormal electrical activity. These irregularities often occur in the areas of the brain responsible for pain processing and sensory perception, such as the trigeminal nerve and the brainstem.
Triggers such as stress, hormonal changes, certain foods, or environmental factors can disrupt the delicate balance of neural activity, leading to hyperexcitability in these key regions. This hyperexcitability can then initiate a cascade of events that ultimately result in the onset of a migraine headache.
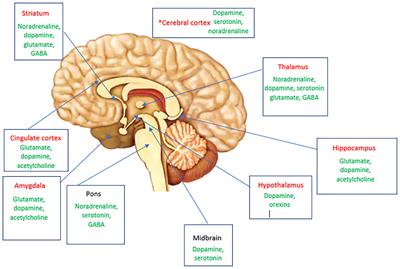
The Role Of Neurotransmitters In Migraine Pathophysiology
Neurotransmitters, the chemical messengers that facilitate communication between nerve cells, also play a critical role in the pathophysiology of migraines. Specifically, the neurotransmitters serotonin and dopamine have been closely linked to migraine attacks.
Serotonin, often referred to as the “feel-good” neurotransmitter, is involved in the regulation of pain perception, mood, and sleep. Studies have shown that low levels of serotonin during a migraine attack can trigger a series of events that result in blood vessel dilation and inflammation, leading to the characteristic throbbing pain experienced by migraine sufferers.
In contrast, dopamine, a neurotransmitter associated with reward and pleasure, may also contribute to migraines. Alterations in dopamine levels have been found in individuals with migraines, indicating that an imbalance in this neurotransmitter system may influence the susceptibility to migraine attacks.
Migraine Aura And Its Neurological Basis
A migraine aura is a series of sensory disturbances that can occur before or during a migraine attack. These disturbances may include visual changes, such as flashing lights or blind spots, as well as sensory symptoms like tingling or numbness.
The neurological basis of migraine aura stems from a phenomenon known as cortical spreading depression (CSD). CSD involves a wave of hyperactivity followed by a period of decreased neural activity that spreads across the cerebral cortex. This wave disrupts normal electrical signalling in the brain, leading to the visual and sensory disturbances associated with migraine aura.
Research suggests that CSD triggers the release of various chemicals and neurotransmitters, including glutamate and calcitonin gene-related peptide (CGRP). The release of these substances further amplifies the cascade of events that contribute to the characteristic pain and other symptoms experienced during a migraine attack.
In Conclusion
The neurological causes of migraine pain are complex and multifaceted. Abnormal brain activity, neurotransmitter imbalances, and the phenomenon of migraine aura all play significant roles in the pathophysiology of migraines. By unravelling these intricate neurological mechanisms, researchers strive to develop more effective treatments and interventions that can provide relief and improve the quality of life for individuals living with migraines.
Vascular Causes Of Migraine Pain
Migraine pain can be triggered by various factors, and one of the significant contributors to this debilitating condition is vascular causes. Understanding the role of blood vessel dilation, cerebral blood flow abnormalities, and the involvement of the trigeminal nerve can shed light on the mechanisms behind migraine pain. This article will delve into these vascular causes in detail, providing insight into the complex nature of migraines and how they affect individuals.
Blood Vessel Dilation And Migraines
In the context of migraines, blood vessel dilation plays a crucial role. When certain triggers, such as stress, hormones, or environmental factors, activate the trigeminal nerve, it sends signals to the blood vessels in the brain. As a result, these blood vessels expand, causing inflammation and congestion.
This dilation of blood vessels can generate immense pressure on the nerves, leading to the throbbing pain commonly associated with migraines. Moreover, the increased blood flow can trigger the release of neuropeptides, which further contribute to the persistence and intensity of the pain.
Cerebral Blood Flow Abnormalities And Migraines
Cerebral blood flow abnormalities are another vascular cause of migraines. Studies have shown that individuals experiencing migraines often exhibit deviations in the regulation of blood flow to the brain. During a migraine attack, there seems to be an altered balance between vasoconstriction (narrowing) and vasodilation (widening) of blood vessels.
These irregularities in cerebral blood flow can impact the delivery of oxygen and nutrients to the brain, triggering the onset of migraine symptoms. The exact mechanisms underlying these abnormalities are still being researched, but understanding this aspect can aid in developing more targeted treatments for migraines.
The Role Of The Trigeminal Nerve In Migraine Pain
The trigeminal nerve, responsible for relaying sensory information from the face and head to the brain, plays a significant role in migraine pain. When the trigeminal nerve becomes activated, it releases chemicals that not only cause blood vessels to dilate but also result in neurogenic inflammation.
This neurogenic inflammation can heighten sensitivity to pain, intensifying the migraine experience. Moreover, the trigeminal nerve can trigger the release of neurotransmitters, such as substance P and calcitonin gene-related peptide (CGRP), which further contribute to the transmission of pain signals.
Understanding the involvement of the trigeminal nerve helps explain why certain triggers, such as bright lights, loud noises, or strong odours, can exacerbate migraine pain. By addressing the underlying mechanisms related to this nerve’s activation, researchers aim to develop more effective treatments and preventative measures for migraines.
Inflammatory Factors And Migraine Pain
Inflammatory factors can contribute to the onset of migraine pain. Understanding these causes is crucial for effective management and treatment of migraines. By recognizing and addressing inflammation, individuals can potentially reduce the frequency and severity of their migraine episodes.
Migraines can be incredibly debilitating, causing throbbing pain, sensitivity to light and sound, and even nausea. While the exact causes of migraines are still not fully understood, emerging research suggests that inflammatory factors play a significant role in the development and intensity of migraine pain.
Inflammation And Its Effect On Migraines
Inflammation is the body’s natural response to injury or infection. It is a protective mechanism triggered by the immune system to remove harmful stimuli and initiate the healing process. In the context of migraines, inflammation can occur in the blood vessels and tissues of the brain, leading to the characteristic pain experienced by migraine sufferers.
Studies have shown that certain inflammatory markers, such as cytokines and prostaglandins, are elevated during migraine attacks. These substances can cause the blood vessels in the brain to dilate and become more sensitive to pain, contributing to the intense throbbing sensation often associated with migraines.
Chronic Inflammation And Migraine Frequency
While inflammation can occur as a response to a specific trigger, such as a food intolerance or environmental allergens, some individuals may experience chronic inflammation, leading to more frequent and severe migraines. Chronic inflammation refers to persistent low-grade inflammation that can be caused by factors such as poor diet, stress, lack of sleep, and a sedentary lifestyle.
When the body is constantly in a state of inflammation, it can disrupt the normal functioning of the immune system and increase the likelihood of migraine attacks. Additionally, chronic inflammation can contribute to the development of other migraine triggers, such as hormonal imbalances and changes in neurotransmitter levels.
The Role Of Immune System Dysfunction In Migraines
The immune system plays a crucial role in maintaining overall health and fighting off infections. However, immune system dysfunction can lead to an exaggerated inflammatory response, triggering migraines in susceptible individuals.
Research has suggested that certain immune system abnormalities, such as increased levels of antibodies and activated immune cells, may be present in individuals with migraines. These abnormalities can result in an overactive immune response, leading to chronic inflammation and frequent migraines.
Psychological Factors And Migraine Pain
Psychological factors and migraines are closely intertwined. The impacts of stress, anxiety, and depression have been known to contribute significantly to the occurrence and intensity of migraine pain. Understanding the link between these psychological factors and migraines is crucial in effectively managing and preventing these debilitating headaches.
Stress, Anxiety, And Migraines
Stress and anxiety are often considered major culprits when it comes to triggering migraines. When we experience stress, our body releases hormones that can lead to increased muscle tension, blood vessel constriction, and changes in neurotransmitter levels. These physiological responses can all play a role in triggering migraines. In fact, studies have shown that individuals who are prone to stress and anxiety are more likely to suffer from migraines.
If you find yourself battling stress and anxiety that contribute to your migraines, it is essential to develop effective coping strategies. Taking regular breaks throughout the day, practising relaxation techniques, such as deep breathing or meditation, and engaging in activities that you find enjoyable and stress-relieving can all help reduce the intensity and frequency of migraines caused by stress and anxiety.
The Link Between Depression And Migraines
Depression and migraines often go hand in hand. Research suggests that individuals with a history of depression are more susceptible to experiencing migraines. The relationship between these two conditions is complex and multifaceted. It is believed that certain chemical imbalances in the brain associated with depression can also affect the occurrence and severity of migraines.
If you suffer from both migraines and depression, seeking professional help is essential. Therapies such as cognitive-behavioral therapy (CBT) and medication management can be effective in addressing both conditions and reducing their impact on your daily life. Openly communicating with your healthcare provider about your symptoms and experiences is key to developing a personalized treatment plan.
Coping Strategies For Psychological Triggers Of Migraines
When it comes to managing migraines triggered by psychological factors, implementing coping strategies can be incredibly beneficial. Some effective techniques include:
- Identifying and avoiding triggers: Keeping a migraine diary can help you identify patterns and pinpoint specific triggers. Once you’re aware of your triggers, make an effort to avoid or minimize exposure to them.
- Prioritizing self-care: Taking care of your physical and mental health is crucial in managing migraines. Implementing regular exercise, maintaining a healthy diet, prioritizing sleep, and practising relaxation techniques like mindfulness or yoga can all contribute to keeping migraines at bay.
- Seeking support: Dealing with migraines can be overwhelming, so seeking support from friends, family, or support groups can provide understanding and helpful advice. Don’t hesitate to reach out for the support you need.
- Exploring therapy options: Therapy, such as cognitive-behavioral therapy (CBT), can help you identify and modify negative thought patterns, manage stress, and develop effective coping mechanisms.
By implementing these coping strategies, you can effectively manage the psychological triggers of migraines and reduce their impact on your overall well-being.
Lifestyle Choices And Migraine Pain
Migraine pain can be debilitating and hinder our ability to carry out everyday tasks. While there are various factors that can contribute to migraines, our lifestyle choices play a significant role in their occurrence and severity. By making conscious decisions about our sleep patterns, exercise routines, and dietary habits, we can effectively manage and reduce the frequency of migraine pain.
Sleep Patterns And Migraines
Poor sleep patterns have been found to be a common trigger for migraines. Insufficient sleep, irregular sleep schedules, and disrupted sleep can all contribute to an increased risk of migraines. When we don’t get enough sleep or have irregular sleep patterns, it can disrupt our body’s natural rhythms, leading to imbalances in neurotransmitters and increased sensitivity to pain.
To reduce the likelihood of migraines, it’s essential to establish a consistent sleep routine. Try to go to bed and wake up at the same time every day, even on weekends. Create a calm and soothing environment in your bedroom, ensuring it’s dark, quiet, and at a comfortable temperature. Avoid electronic screens, caffeine, and heavy meals close to bedtime as they can disrupt your sleep cycle.
Exercise And Migraine Frequency
Regular exercise is beneficial for our overall health and well-being, but it can also have an impact on migraine frequency. While exercise can trigger migraines in some individuals, for others, it can provide relief and reduce the frequency of attacks.
Engaging in moderate aerobic exercises such as walking, jogging, or swimming can promote better blood flow and reduce stress levels, which are common triggers for migraines. However, it’s important to start slowly and gradually increase the intensity of the exercise to prevent exertion-induced migraines. Additionally, ensure you stay hydrated before, during, and after exercising to avoid dehydration-triggered migraines.
Impact Of Diet And Hydration On Migraines
The food we eat and our hydration levels can significantly influence the occurrence of migraines. Certain foods and beverages are known migraine triggers, while dehydration can also contribute to their onset.
Keeping a migraine diary can help identify potential dietary triggers. Common culprits include processed foods, aged cheeses, caffeine, alcohol, and artificial sweeteners. It’s best to avoid or limit the consumption of these triggers. Additionally, staying adequately hydrated by drinking enough water throughout the day can help prevent dehydration-induced migraines.
By making conscious lifestyle choices and considering our sleep patterns, exercise routines, and diet, we can mitigate the risk of migraine pain. Implementing these changes may require some adjustment, but the long-term benefits of reduced migraine frequency and severity are worth it.
Treatment Options For Migraine Pain

Migraine pain can be caused by various factors such as hormonal changes, triggers like stress or certain foods, and neurological abnormalities. Treatment options for migraines include lifestyle changes, over-the-counter pain relievers, prescription medications, and alternative therapies like acupuncture. Consulting a healthcare professional can help identify the cause and determine the most suitable treatment plan for managing migraine pain.
Medications For Acute Migraine Relief
When it comes to treating migraine pain, many individuals turn to medications for immediate relief. These medications are specifically designed to target the symptoms of a migraine attack, providing fast and effective relief. Some commonly prescribed medications for acute migraine relief include: 1. Triptans: Triptans are a class of drugs that work by constricting blood vessels and blocking pain signals in the brain. They can help relieve pain, nausea, and sensitivity to light and sound. Examples of triptans include Sumatriptan (Imitrex) and Rizatriptan (Maxalt). 2. Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs such as Ibuprofen (Advil) and Naproxen (Aleve) are commonly used to alleviate the symptoms of a migraine attack. These medications can help reduce inflammation and relieve pain. 3. Analgesics: Analgesics like Acetaminophen (Tylenol) can be effective in relieving mild to moderate migraine pain. These over-the-counter medications can reduce pain without causing significant side effects.
Preventive Treatments For Migraines
In addition to acute migraine relief, preventive treatments are available for individuals who experience frequent or severe migraines. These treatments aim to reduce the frequency and severity of migraine attacks, allowing individuals to better manage their condition. Some commonly used preventive treatments for migraines include: 1. Beta-blockers: Beta-blockers such as Propranolol and Metoprolol are often prescribed to individuals with migraines. These medications work by blocking the effects of adrenaline, reducing the frequency and severity of migraine attacks. 2. Antidepressants: Certain antidepressants, such as Amitriptyline and Venlafaxine, can be effective in preventing migraines. These medications alter the chemical balance in the brain, reducing the occurrence of migraine attacks. 3. Botox injections: Botox injections have been approved by the FDA for the prevention of chronic migraines. This treatment involves injecting Botox into specific muscles of the head and neck to prevent migraines from occurring.
Lifestyle Modifications And Alternative Therapies
Alongside medications and preventive treatments, lifestyle modifications and alternative therapies can also play a crucial role in managing migraine pain. These non-medical approaches can complement traditional treatment methods and help individuals find relief. Some lifestyle modifications and alternative therapies for migraines include: 1. Stress management: Stress is a common trigger for migraines, so learning stress management techniques can be beneficial. This can include regular exercise, relaxation techniques, and maintaining a balanced lifestyle. 2. Dietary changes: Certain foods and beverages, such as aged cheese, chocolate, and caffeine, are known to trigger migraines in some individuals. Identifying and avoiding these triggers can help reduce the frequency and severity of attacks. 3. Acupuncture: Acupuncture is an alternative therapy that involves the insertion of thin needles into specific points of the body. This practice is believed to help rebalance the body’s energy flow and provide relief from migraines. Overall, when it comes to treating migraine pain, a combination of medications, preventive treatments, lifestyle modifications, and alternative therapies can provide effective relief. It is important for individuals to work closely with their healthcare providers to find the most suitable treatment plan for their specific needs.
Frequently Asked Questions For Causes Of Migraine Pain
What Is The Main Cause Of Migraine?
The main cause of migraine is still not fully understood, but it is believed to be a combination of genetic and environmental factors that trigger abnormal brain activity and an overactive nervous system. Researchers also suspect changes in serotonin levels and blood vessels play a role.
How Do You Make A Migraine Stop Hurting?
To stop a migraine from hurting, try taking over-the-counter pain relievers, such as ibuprofen or aspirin. Applying a cold or warm compress to your head may also provide relief. Make sure to rest in a quiet and dark room, and avoid triggers like bright lights and loud noises.
If your migraines persist, consult a healthcare professional for further advice.
What Neurological Disorders Cause Migraines?
Neurological disorders that cause migraines include migraines with aura, hemiplegic migraine, and vestibular migraines. Migraine with aura involves visual disturbances, while hemiplegic migraine presents with temporary paralysis. Vestibular migraine affects balance and coordination. These disorders result in recurrent, severe headaches.
What’s The Difference Between A Headache And A Migraine?
A headache is a general pain in the head, while a migraine is a recurring and severe headache that can cause other symptoms like nausea and sensitivity to light and sound.
What Are The Common Triggers For Migraine Pain?
Migraine pain can be triggered by various factors such as stress, certain foods, hormonal changes, and sleep disturbances.
Conclusion
Understanding the causes of migraine pain is crucial for effective treatment and prevention. By identifying triggers such as stress, hormonal changes, certain foods, and environmental factors, individuals can take proactive steps to manage their migraines. Additionally, lifestyle modifications, stress reduction techniques, and appropriate medication can help alleviate the severity and frequency of migraine attacks.
With this knowledge, individuals can regain control over their lives and experience relief from debilitating migraines.








Be First to Comment